Intrauterine insemination is the deposition of washed and capacitated sperm into
the uterine cavity and remains one of the most popular ART techniques for patients
with mild endometriosis, low sperm counts, poor sperm motility, greater percentage
of abnormal sperms, sexual dysfunction (faulty technique or inadequate deposition
of sperm in the vagina), some cases of one sided tubal block, polycystic ovaries
and also those with unexplained infertility.
IUI is not for every couple and case selection is important to maintain optimal
success rates with this treatment modality. For example, IUI is unlikely to work
if the tubes are damaged or there is moderate to severe endometriosis or the sperm
counts and motility are very poor. So also, it is not too successful in women above
the age of 35 with an already depleted egg reserve as indicated by an AMH level
of < 2 ng/ml.
To enhance the success rate we need the following criteria / investigations
Age < 35 years
Duration of infertility < 5
years
Serum AMH > 2
Serum FSH < 8
Sperm wash yielding adequate
high speed sperm in a case of sperm problems.
HSG or Laparoscopy showing
one normal and open tube.
Transvaginal ultrasound showing
normal uterus and ovaries (polycystic is acceptable).
Also, we need to stimulate the ovaries of the wife to get more eggs, improve the
quality of eggs, enhance the lining of the uterus and be able to time the insemination
perfectly with injections
Ovarian Stimulation for IUI
One of the easiest and most cost effective protocols for COHS in IUI is the Clomiphene (CC) / Letrozole -IUI protocol - Tablets of CC or Letrozole are administered once daily from day 2 or 3 of menses - Transvaginal USG follicular monitoring being performed daily from day 7 of cycle until the lead follicle (Egg) reaches 17 - 18 mm in mean diameter and endometrium (lining of the uterus) reaches thickness of > 8 mm when 5000-10000 IU of hCG (ovulation trigger injection) is administered and IUI is performed at 40 hours post hCG. Luteal phase support is with micronized progesterone vaginal capsules 200 mg twice a day.
Letrozole - HUMAN MENOPAUSAL GONADOTROPIN (HMG):
Letrozole is administered in a dose of 2.5 mg twice daily from days 3 - 7 of menses. Inj hMG 150 IU is then administered from day 7/8 of cycle on a daily basis until the lead follicle reaches 17 - 18 mm in mean diameter. hCG 5000-10000 units is administered on that day and IUI performed on 2 days thereafter.
Follicle stimulating hormone (FSH)-IUI:
After a baseline scan on day 2 to ensure endometrial shedding and no residual ovarian
cysts, Injections of FSH 75-150 IU are administered Intramuscularly daily. Ultrasound
monitoring is started on day 6. If there are more than 3 follicles 12 mm in mean
diameter, the same dose is continued. If less than 3 follicles 12 mm in diameter,
the dose might be increased to 225 IU per day. The ovulation trigger of hCG 5000-10000
IU is then administered when the lead follicle reaches 18 mm in mean diameter followed
by IUI on two days thereafter.
Agonist / Antagonist: Sometimes, doctor might combine a GnRh agonist
or antagonist (Cetrorelix or Ganirelix) with the FSH stimulation for enhancing the results and better timing
of ovulation. This would help 20% of patients where the follicles did not rupture
or became cysts in previous cycles
Sperm Preparation for IUI
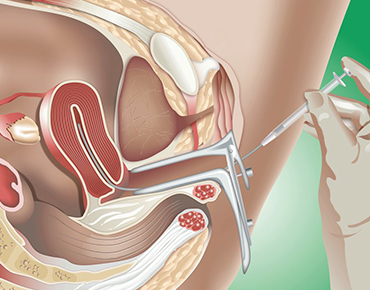
The sperm is prepared in the semen laboratory by either of two methods, namely layering
or gradient and the final washed sperm is then loaded in a catheter and transferred
to the womb (IUI).
Results
The average success rate of IUI per cycle is 5-30 % depending upon the indication
and the COHS protocol used.
Number of Cycles
The normal recommendations are 2-3 cycles of IUI prior to resort to more aggressive ART such as IVF & ICSI. For the unexplained infertility group, current recommendations are one cycle of L-hMG-hCG-IUI, followed by one cycle of Pure FSH-hMG-IUI followed by one cycle of FSH-IUI with agonist or antagonist.
Advisory Note
With modern day IVF being too successful, it would be wise to undergo not more than
3 cycles of IUI. Remember that the success rate with IUI using husband's sperm is
@ 15-25 % and with donor sperm is @ 30 % owing to the limitations of the technique.
In cases of unexplained infertility please remember that most of them suffer from
infertility owing to failure of the sperm to fertilize the egg (inability to pierce
the tough shell of the egg). This cannot be proved by any known test and therefore
the couple is labelled as having "Unexplained infertility" and often told that all
is well and it is just a matter of time before they achieve pregnancy. Currently,
we are not in favour of this school of thought and prefer more aggressive treatment
such as ICSI-IVF (where the sperm is injected into the egg in the laboratory) to
achieve pregnancy, especially after 2-3 attempts at IUI have failed.